
A Complete Guide to HIPAA EDI Transactions: What They Are and How They Work
Healthcare runs on data, whether it is insurance claims, eligibility checks, or payment details. All of this crucial data needs to move quickly and securely between providers, insurers, and third parties.
However, without standardized processes, managing all these streams of information can become challenging.
That’s where HIPAA EDI transactions come in.
They ensure that sensitive patient information is exchanged efficiently while staying compliant with HIPAA regulations. More than just a requirement, these transactions help ensure timely communication, accurate data exchange, and faster processes. All of this ensures timely and effective care delivery to the patients.
Let’s discuss the different types of HIPAA EDI transactions, their role in modern healthcare, and how they’re driving smoother, more secure operations across the industry.
What is HIPAA EDI?
The Health Insurance Portability and Accountability Act (HIPAA), established in 1996, is designed to keep individual health information private. This act introduced HIPAA EDI (Electronic Data Interchange) Standards to secure electronic health data sharing among healthcare providers, insurers, and related entities.
Healthcare EDI sets the rules for how data should be formatted when electronically exchanged between different stakeholders to ensure secure and efficient communication and reduce manual tasks.
EDI allows healthcare providers and insurance companies to electronically manage tasks like billing, claims processing, and record-keeping, making these processes smoother while complying with HIPAA rules.
How Are EDI and HIPAA Related?
EDI and HIPAA are interconnected and work closely to ensure the secure exchange of data, improvement in healthcare operations, and uninterrupted flow of information between various parties.
Imagine a healthcare provider seamlessly submitting insurance claims, receiving quick approvals, and getting paid without delays. That’s the power of HIPAA-compliant EDI transactions.
For instance, by using EDI 837 for claims and EDI 835 for remittances, healthcare providers can automate data exchanges, reduce administrative work, and speed up reimbursements.
Plus, instead of dealing with manual paperwork or tracking down errors, billing teams can focus on tasks that can improve efficiency and patient care.
Secure Data Exchange
EDI supports the secure sending of healthcare data using encryption methods like SSL (Secure Sockets Layer), VPN (Virtual Private Network), or even a US proxy to route data securely within regional compliance frameworks. This encryption keeps patient data safe from unauthorized access while it’s being sent. It also ensures seamless communication between healthcare providers and insurance companies using secure protocols like AS2 and SFTP.
Using EDI for sending sensitive data helps healthcare organizations reduce the risk of data breaches and meet the requirements of the HIPAA Security Rule. The HIPAA rule ensures patient information stays private and safe throughout the exchange process.
Smooth Healthcare Operations
EDI makes healthcare operations more efficient by automating processing claims and checking eligibility. For example, when a claim is sent electronically through EDI, the system automatically checks the data for errors and confirms the patient’s eligibility for coverage. This automation speeds up reimbursements and reduces errors that could cause claim denials or delays.
EDI allows for instant communication between healthcare providers, insurers, and others. This quick information exchange improves coordination and speeds up decisions.
Transform Your Healthcare Operations with HealthEDI
Discover how HealthEDI transforms healthcare operations with secure, efficient data exchanges. Automate billing, claims processing, and more while safeguarding patient privacy. Learn about our HIPAA-compliant solution for seamless integration and compliance today.
Speak to Our TeamWhat Is the HIPAA EDI Document Standard?
The HIPAA EDI standard is a set of rules specifying the format for data transmission. It ensures that everyone, from healthcare providers to insurance companies, understands and uses the same process when sharing patient records or insurance claims.
This EDI standard focuses on protecting patients’ information by using electronic secure formats like digital encryptions. It also speeds up the process compared to handling paperwork, as automation allows faster transmission and processing of healthcare transactions.
The HIPAA EDI standard often uses X12N, a standardized language with specific rules for structuring information like patient ID numbers and service codes. This standardization ensures that all healthcare providers and insurers understand each other clearly and securely.
Components of EDI Transaction Set
The American National Standards Institute (ANSI) has developed the ASC X12, or simply X12, standards for different industries. Currently, over 300 X12 EDI standards exist, covering sectors like insurance, healthcare, transportation, and retail.
Each EDI type or set is identified by a unique three-digit code. EDI documents, also known as transaction sets, organize data in a specific way.
These documents consist of three main parts:
1. Data Elements
These are the basic units of information, like the name of a company or how many items are being bought. EDI standards help define data elements, including their size limits and possible values, such as types of currency.
2. Segments
These are groups of related data elements. They are identified by a unique segment ID, like the date of birth. Some segments must always be included, while others depend on what information needs to be conveyed.
3. Sets (Transaction Sets)
Sets, or envelopes, organize the transaction sets for sending data. Each envelope starts with a header segment, includes a digital marking control number for identification, and ends with a segment that indicates the end.
How HIPAA EDI Transactions Work
HIPAA standards ensure that all EDI transactions follow the same steps. Let’s have a look at how a typical HIPAA-compliant EDI transaction works with the help of a EDI 837 (Claim Submission) transaction workflow:
Step 1: Data Collection
- A healthcare provider (doctor, hospital, or clinic) delivers a service to a patient.
- The provider’s system then gathers all the necessary details: patient demographics, diagnosis codes, treatment details, and billing information.
Step 2: EDI File Creation
- The provider’s EDI management system converts this information into a HIPAA-compliant transaction file (Claim Submission format).
Step 3: Transmission via EDI Network
- The EDI file is sent securely over an EDI network.
- The file is validated for errors, and the system ensures compliance with payer requirements.
Step 4: Payer Receives and Processes the Claim
- The insurance payer (e.g., Medicare, private insurer) receives the claim.
- It is automatically checked for errors, eligibility, and policy coverage.
- If needed, the payer may send a 277 Claim Acknowledgment to confirm receipt or flag issues.
Step 5: Claim Approval & Payment Processing
- If the claim is approved, the payer generates an 835 Electronic Remittance Advice (ERA) detailing payment and adjustments.
- The payment is sent electronically to the provider’s bank account.
Step 6: Provider Reconciles Payment
- The provider receives the 835 Remittance Advice and updates their records accordingly.
- If needed, they can submit a claim status inquiry (276/277 transaction) or an appeal for denied claims.
Benefits of HIPAA-Compliant EDI Transactions
While it may seem like the process described above is a lengthy one, the use of EDI in this workflow helps in multiple ways, such as:
- Facilitating faster processing, which reduces claim approval time from weeks to days,
- Automated validation minimizes claim rejections thanks to fewer errors.
- Extensive cost savings due to the elimination of paper-based submissions and manual data entry work.
- Seamless HIPAA-compliant data exchange.
The same workflow also applies to other transactions, including eligibility checks, payments, and authorizations, which makes EDI critical for efficient healthcare administration.
The 10 Most Important HIPAA EDI Transaction Sets
HIPAA requires that all healthcare providers follow specific EDI standards to dispatch protected information like claims, check eligibility/reimbursement, and provide payment instructions. This standard ensures secure and standardized transmission of data. Organizations in the healthcare industry use multiple EDI transaction sets.
1. 837 Healthcare Claim Transaction Set
Healthcare providers use the EDI 837 Health Care Claim Transaction Set to send billing and service information for all healthcare claims, except for retail pharmacy claims. They can send these details directly to insurance companies or through billing services and claims processing centers. The system also helps manage claims and payments between insurance companies when patients have multiple insurers. This transaction set aids in reporting to government agencies that monitor healthcare billing and payments, making submitting and tracking healthcare claims easier.
2. 835 Healthcare Claim/Payment/Advice Transaction Set
Through the Healthcare Claim Payment/Advice Transaction Set, insurers pay healthcare providers and send Explanation of Benefits (EOB) and remittance advice.
3. 834 Health Insurance Exchange Enrollment Transaction Set
The EDI 834 Benefits Enrollment and Maintenance Set allows employers, unions, government agencies, insurance agencies, associations, or healthcare organizations to enroll members in benefit plans.
4. 820 Payroll Deducted and Other Group Premium Payment for Insurance Products Transaction Set
The Payroll Deducted and Other Group Premium Payment for Insurance Products transaction facilitates premium payments and sends information to financial organizations.
5. 270 Healthcare Benefit Eligibility/Inquiry Transaction Set
Healthcare institutions use the Healthcare Eligibility/Benefit Inquiry to ask about benefits and subscriber eligibility.
6. 271 Healthcare Benefit Eligibility Response Transaction Set
The Healthcare Eligibility/Benefit Response replies to healthcare benefits and eligibility inquiries.
7. 276 Claim Status Request Transaction Set
Healthcare providers use the Healthcare Claim Status Request to check the status of healthcare claims submitted to an insurer.
8. 277 Status Request Response Transaction Set
The Healthcare Claim Status Notification allows healthcare payers or their agents to update providers, patients, or their agents about the status of a healthcare claim and request more information. This method doesn’t replace the payment advice process and doesn’t manage payment postings. Notifications can detail overall summaries or specific services and may be given when requested.
9. 278 Healthcare Review Transaction Set
Hospitals use the Healthcare Service Review Information (278) to request service authorization from an insurer.
10. 997/999 Implementation Acknowledgment Transaction Set
This transaction set is important for acknowledging the outcome of analyzing electronic documents’ syntax, even though the HIPAA laws don’t specifically list it. It’s essential for X12 transaction sets, organized into groups for business data interchange. But this set needs to explain the meanings of the information in these documents.
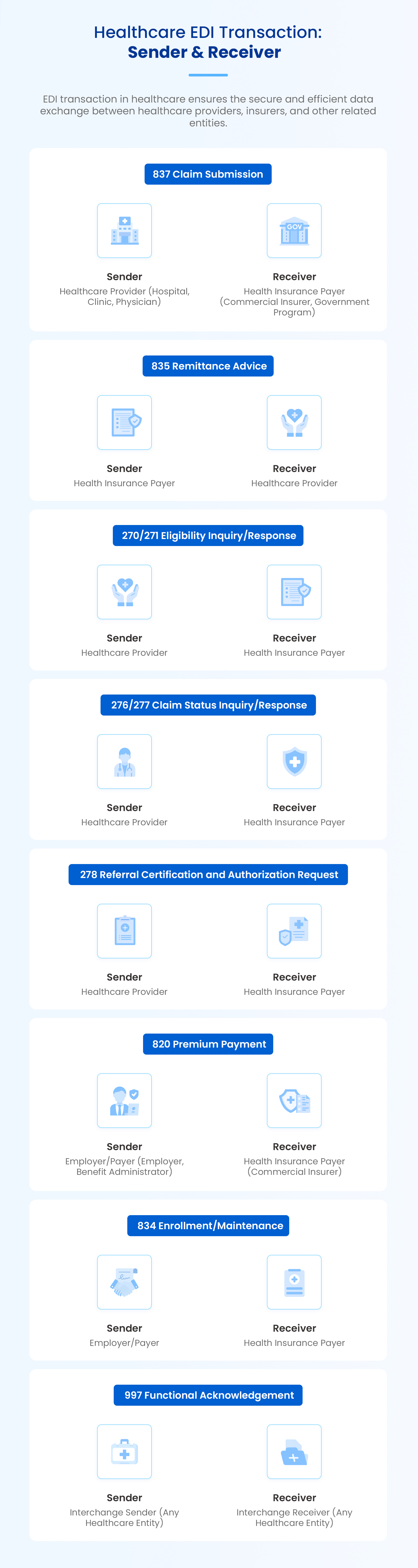
Healthcare EDI Transaction: Sender & Receiver
EDI transactions in healthcare ensure the secure and efficient data exchange between healthcare providers, insurers, and other related entities. Let’s look at the sender and receiver for each of these documents:
Overcoming Challenges in HIPAA EDI Transactions
While HIPAA EDI transactions offer a structured and secure way to exchange healthcare data, making the most of them requires having the right healthcare EDI management strategy.
Here are key focus areas to ensure a smooth and efficient implementation:
- Ensuring Compliance: HIPAA guidelines provide a clear framework for handling sensitive data. Using an EDI solution designed for HIPAA compliance helps organizations effortlessly align with security and privacy best practices.
- Maintaining Data Accuracy: Consistently accurate data leads to streamlined claims processing and faster reimbursements. EDI solutions with automated validation features verify inputs before submission, ensuring smooth transactions.
- Seamless System Integration: EDI transaction processing requires connecting with existing EHR, billing, and claims management systems while also integrating smoothly with partners. An EDI software that can integrate seamlessly with internal systems and connect with external data sources can enhance efficiency and reduce manual work.
- Enhancing Security Measures: Secure data exchange protocols like AS2, SFTP, and VPNs safeguard patient information while maintaining HIPAA standards.
- Optimizing EDI Transaction Workflows: Real-time tracking and proactive monitoring enable quick resolution of any processing delays, ensuring that transactions run smoothly and efficiently.
Best Practices for HIPAA EDI Transactions
Organizations can maximize the benefits of HIPAA EDI transactions by adopting certain best practices, such as:
- Use a HIPAA-Compliant EDI Solution: A dedicated EDI platform simplifies compliance, automates workflows, and ensures secure data transmission.
- Automate Data Validation: Built-in validation checks improve accuracy, allowing transactions to be processed efficiently with minimal adjustments.
- Seamless Integration Features: Selecting an EDI system that seamlessly connects with existing healthcare applications enhances overall workflow efficiency.
By focusing on these strategies, healthcare organizations can fully harness the power of HIPAA EDI transactions, leading to faster processes, enhanced accuracy, and seamless data exchange.
Execute HIPAA EDI Transactions Smoothly with HealthEDI
HIPAA EDI transactions offer clear benefits. They enable the secure transfer of sensitive patient data, benefiting patients and healthcare professionals. HIPAA EDI also ensures compliance with regulations and other laws and streamlines healthcare communication.
The best way to experience these advantages is to leverage software that automates managing EDI transactions, which can save valuable time and resources while ensuring continued accuracy and security.
HealthEDI provides a secure environment for exchanging data, transforming it into a usable format, and ensuring its accuracy. It facilitates the secure healthcare data exchange using HIPAA-compliant X12X5010 and HL7 standards. This allows hospitals, labs, and doctors to electronically share vital information like lab results, medical records, and patient admission details.
The healthcare EDI processing solution automates the process of loading, validating, and transforming data following industry standards like X12, EDIFACT, or HL7. It also allows organizations to create EDI messages that strictly adhere to these standards, guaranteeing that partners understand them.
Schedule a demo today to maintain consistency and reliable execution of EDI transactions.
What is HIPAA EDI, and why is it important?
What are the key types of HIPAA EDI transactions?
HIPAA defines several EDI transaction sets for different healthcare processes. Some of the most commonly used ones include:
EDI 837 – Healthcare claim submission
EDI 835 – Payment and remittance advice
EDI 270/271 – Eligibility inquiry and response
EDI 276/277 – Claim status inquiry and response
EDI 278 – Service authorization request
Each transaction type ensures that healthcare data is exchanged in a standardized, structured format.
 Astera AI Agent Builder - First Look Coming Soon!
Astera AI Agent Builder - First Look Coming Soon!
