Insurance Claims Management: A Comprehensive Guide
The insurance industry is a data-intensive sector. Insurers collect and analyze vast amounts of data to assess risk, underwrite policies, and manage claims. However, manually processing this data can be time-consuming, error-prone, and costly. That’s why many insurers are turning to contemporary data extraction solutions to automate the insurance claims management process.
In this article, we will explore how modern-day data extraction tools enable insurers to streamline insurance claims management, reduce costs, and improve customer satisfaction.

What is Claims Management in Insurance?
Claims management in insurance refers to the process of handling and settling insurance claims made by policyholders. When a policyholder experiences a loss or damage covered by their insurance policy, they file a claim with their insurance company. The company then processes the claim and disburses the necessary amount if the claim is valid.
Efficient claims management is essential for insurance companies to fulfill their obligations to policyholders promptly and fairly while also minimizing fraud and managing costs.
Why is There a Need For Automating Insurance Claims Management
Managing claims involves hundreds of documents. Around 3.5 million claims done are filed each year in the US – and that’s just homeowner claims. If we include car claims, health insurance claims, and others, the number is much bigger.
The typical management process involves a claims analyst processing each of these claims one-by-one. Some of the documents can take a lot of time to process through this approach: communication breakdown, large amount of data, and administrative burdens. The image below highlights the costs for common transactions.
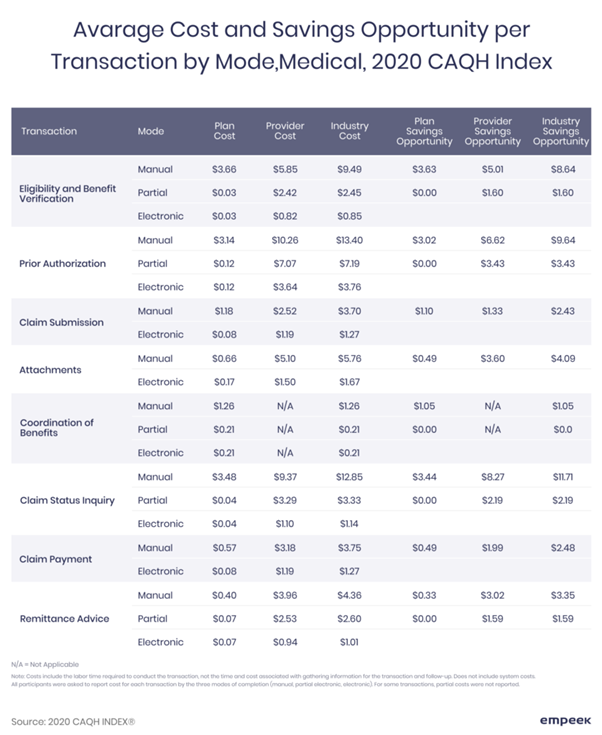
There is great potential here in removing inefficiencies across these transactions. Automation can be a game changer here. A McKinsey report states that automating the claims process can help reduce costs by 30%. Not only can it help internally, it can also improve a firm’s competitiveness: only 5% of insurance companies currently utilize automation to review claims.
One way of innovating claims management in insurance is through data extraction tools. A growing number of insurance companies are using these tools to streamline their document management.
The Role of Advanced Tools in Insurance Claims Management
AI-powered tools can automate claims management by intelligently extracting relevant information from various documents, such as insurance claim forms, medical records, and police reports, and convert it into structured data that can be easily processed by computer systems. This not only speeds up the claims processing time but also ensures accuracy and consistency in data.
Moreover, these tools can also help insurers identify fraudulent claims by flagging inconsistencies in data. For example, if a claimant reports an injury that is not consistent with medical records, the data extraction tool can detect it. The tool can then alert the insurer to investigate the claim further.
Leveraging Cutting-edge Technologies for Improving Insurance Claims Management
Modern-day tools employ several technologies to instantly extract data from insurance claims, including:
- Optical Character Recognition (OCR)
OCR involves scanning and digitizing physical documents, such as claim forms and receipts, and converting them into machine-readable text. OCR is useful when dealing with structured data, such as form fields. It can recognize specific characters and extract them automatically.
- Natural Language Processing (NLP)
NLP involves analyzing unstructured text, such as medical reports and police reports, to extract relevant information. NLP algorithms can recognize patterns and relationships between words and phrases, allowing them to extract meaning from text data. - Machine learning (ML)
ML involves training algorithms to recognize patterns and relationships in data, allowing them to extract information automatically. Machine learning algorithms can analyze large datasets and learn from them over time, improving their accuracy and efficiency. - AI Template-based Data Extraction
Template-based data extraction is a technique that uses pre-defined templates to identify specific data fields in different types of documents. These templates are created using machine learning algorithms, enabling them to extract data fields with high accuracy. AI Template-based data extraction provides unparalleled accuracy, ensuring that 100% of relevant data is extracted when implemented correctly.
Benefits of Automating Insurance Claims Management
Automating insurance claims management processes can provide several benefits to insurers, such as:
- Faster claims processing times: By automating the data entry process, insurance firms can reduce the time it takes to process claims, allowing them to provide faster payouts to their customers.
- Cost savings: By reducing manual labor and errors, claims management software can help insurers reduce their operational costs and improve their bottom line.
- Improved customer satisfaction: By providing faster claims processing times and reducing the need for manual paperwork, these tools can improve customer satisfaction and loyalty.
Practical Scenarios: Insurance Claims Management Use Cases
Auto Insurance Claims:
In the case of auto insurance claims, the process of filing a claim can be time-consuming and complicated. Customers need to submit claim forms, repair estimates, and other supporting documents, which can take several days to process.
By using OCR to scan and digitize these documents, insurers can automate the data entry process and extract relevant information, such as the type of damage, cost of repair, and date of the accident.
Consider a scenario where a customer submits a claim for a fender-bender accident. In this situation, the OCR system can scan and extract relevant information from the repair estimate. It can identify details such as the cost of replacing the damaged part and the estimated time required to complete the repair.
This information can then be entered into the insurer’s system automatically, reducing the time it takes to process the claim and ensuring that accurate and consistent data is entered into the system.
Health Insurance Claims:
Health insurance claims can be complex and time-consuming. Claimants need to provide medical records, bills, and other supporting documents to prove that they are eligible for coverage. By using NLP to analyze medical records, insurers can extract relevant information, such as the diagnosis, treatment, and medication prescribed. This can improve the claims processing time and accuracy.
For example, if a claimant submits a medical bill for a surgery, the NLP system can extract information from the bill, such as the date of the procedure, the name of the physician, and the type of surgery performed. This information can then be used to determine the appropriate payout amount and ensure that the claim is processed accurately and quickly, which can improve customer satisfaction.
Workers’ Compensation Claims:
Workers’ compensation claims can be complex, as they involve medical bills, reports, and other supporting documents. By using OCR to scan and digitize these documents, insurers can automate the data entry process. They can extract relevant information, such as the date of treatment, type of injury, and cost of treatment.
For example, if a claimant submits a medical bill for a work-related injury, the OCR system can extract information from the bill, such as the date of treatment, the type of injury sustained, and the cost of treatment.
Streamline Claims Management with Astera
Modern-day data extraction tools offer significant benefits to the insurance industry by streamlining claims management processes, reducing costs, and improving customer satisfaction.
Therefore, it is imperative to invest in the right claims processing tool. Astera, a leading data extraction solution, can help greatly streamline claim processing for firms.
Astera has helped Aclaimant, an advanced risk reduction and incident management system, reduce claims management time by 50%. The customer was able to extract claims data from PDF forms into excel and CSV using pre-built templates. They were then able to set up an automation process for all incoming files, enabling them to reduce time-to-insight significantly.
In addition to data extraction, Astera provides an end-to-end platform for claims processing. It helps users clean data, orchestrate ETL/ELT pipelines, and build a custom data warehouse. All without writing any code.
Try it for yourself with a free 14-day trial or get in touch with us for a personalized demo!
Revolutionize Insurance Claims Management with Astera ReportMiner
Optimize your claims management with Astera ReportMiner's no-code data extraction and automation. Speed up processing, boost accuracy, and improve customer satisfaction by automating workflows—without writing any code.
Book a Demo or Get a 14-day Free Trial! Astera AI Agent Builder - First Look Coming Soon!
Astera AI Agent Builder - First Look Coming Soon!