Streamlining Prior Authorization with EDI 278: Minimizing Costs, Delays, and Provider Burnout
Manual prior authorization (PA) is a critical step for medical coverage approval but is notoriously time-intensive, with physicians spending an average of 41 hours weekly to process these requests. This not only leads to provider burn out but delays caused by manual prior authorization an also impact patient care. To address this, legislation in over 30 states in 2023 advocates for a shift to electronic PA processes.
PA requests surged by 61% after lifting COVID-19 restrictions, yet a staggering 72% are still manually processed. The Electronic Data Interchange (EDI) 278 transaction set is designed to overhaul these outdated practices, offering a solution that cuts down on claim rejections, streamlines workflows, prevents delays in patient care, and reduces provider burnout, leading to overall improved healthcare delivery
The Challenges:
Delays in Patient Care
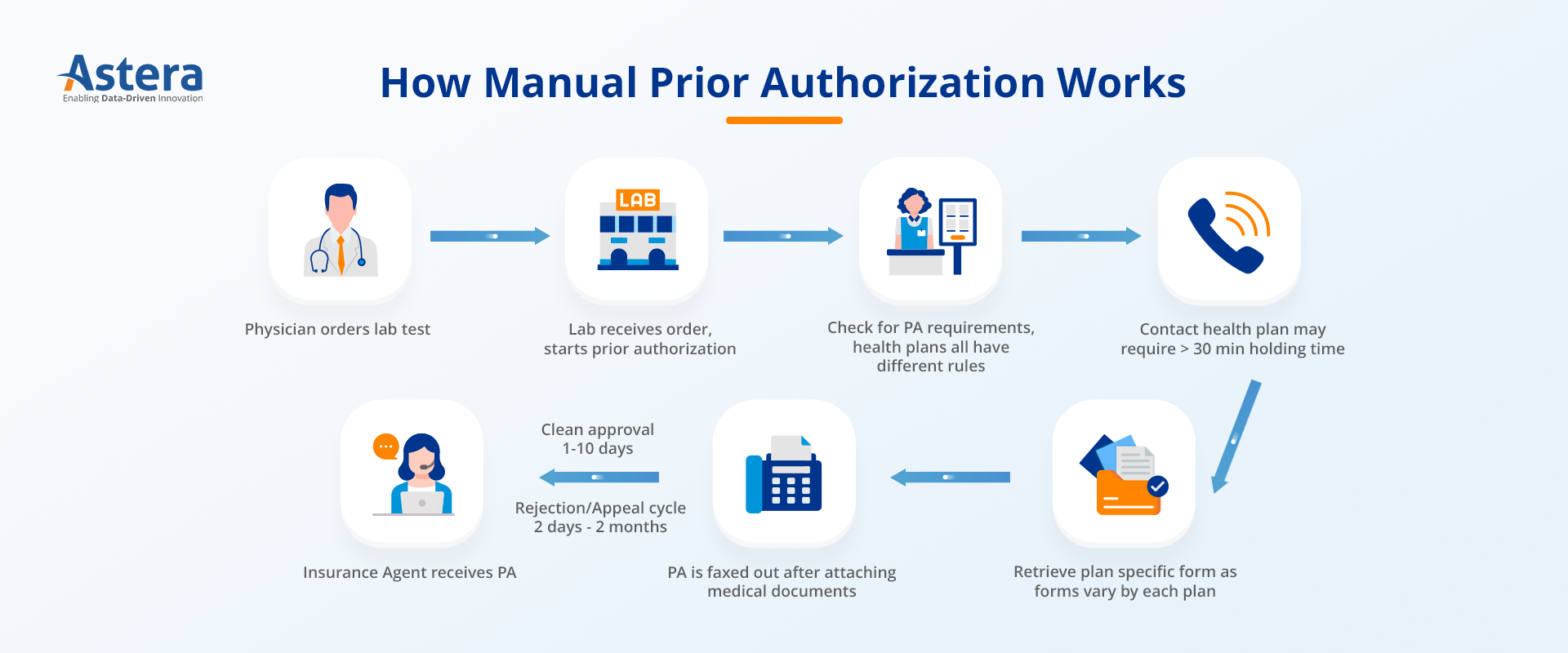
In the traditional system, a patient’s urgent need for medication is met with a slow, manual prior authorization (PA) process. Healthcare providers send PA requests via fax, which then undergoes a lengthy review by the insurance provider, involving multiple departments and often requiring additional information. On average, manual PA requests can take anywhere from one day to one month to complete, due to varying requirements across payers. Such delays can have a significant impact on patient health outcomes.
According to a survey of healthcare providers, 94% believe that PA restrictions cause delays in accessing necessary care. 89% of respondents believe PA delays have a negative impact on patient clinical outcomes. Likewise, 82% of doctors said prior authorization sometimes leads to patients abandoning a recommended course of treatment.
Provider Burnout
Prior authorization often involves complex administrative tasks, such as manually filling out forms, gathering supporting documentation, and submitting requests through multiple channels. Physicians, on average, handle 45 PA requests per week, creating significant administrative burdens and contributing to provider burnout.
Claim Denials
Approximately 80% of denied claims result from a lack of authorization or improper requests, creating significant financial burdens for providers. Streamlining prior authorization can help providers reduce claim denials.
Increasing Cost amongst PA Surge
Prior authorization has garnered attention for its inefficiencies, delays, and administrative burdens, but the cost of processing these requests manually has also increased over the years. Manual data entry, paper-based workflows, errors or duplications of various degrees contribute to increased during in prior authorization. The recent surge in PA requests has exacerbated the issue, leading to even higher administrative spending.
EDI 278’s Role in Enhancing Prior Authorization Workflows
EDI 278 replaces manual processes with electronic transactions, streamlining and enhancing prior authorization (PA) workflows in the healthcare industry.
Streamlining Response Times
EDI 278 replaces manual processes, such as faxing PA requests and waiting up to a month for approval, with electronic submissions. This allows healthcare providers to submit requests directly to the insurer’s system, where they are automatically directed to the correct department for processing. According to the CAQH Index 2022, EDI 278 requests take 11 minutes less to process compared to manual PA requests, potentially saving providers up to 35.36 hours per physician each month.
Improving Patient Care
EDI 278 ensures the request is automatically and efficiently routed to the correct department within the insurer’s system. With EDI 278, insurers too can automate their workflows and process requests more quickly, enabling them to respond to PA requests within hours instead of days or months.
The impact of this swift process is profound. Patients can get the treatment they need approved on the same day, thereby improving their chances of a better health outcome.
Reducing Administrative Burden
EDI 278 automates prior authorization requests processes by automating electronic data entry and document submission. This automation significantly reduces administrative burdens on providers. As a result, healthcare providers experience a significant reduction in manual work, freeing up valuable time and resources to focus on patient care. Additionally, it helps reduce provider burnout.
Increasing Accuracy
EDI 278 ensures the accuracy and completeness of information in PA requests, reducing the chance of claim denials. Providers and payers can send and receive authorization requests promptly, leading to early resolution of issues.
Saving Time and Costs
PA workflows enabled by EDI 278 can help providers save time and resources and avoid unnecessary costs. EDI 278 eliminates the need for manual data entry, reducing paperwork and the potential for errors. According to an HFMA study, EDI 278 is 5.25 times faster than manual PA requests and twice as fast as web portal processing. Likewise, according to the CAQH Index 2022, organizations can save up to $645 million annually by transitioning from manual workflows.
Transforming Prior Authorization with Astera EDIConnect
With the ever-increasing demand for efficient prior authorization in US healthcare, EDI 278 has emerged as a game-changer, replacing cumbersome manual processes. By streamlining workflows, automating administrative tasks, and enhancing data accuracy, EDI 278 reduces delays and lowers operational expenses, ultimately improving patient care and financial outcomes.
In this landscape, Astera EDIConnect takes the stage as a comprehensive solution, empowering healthcare organizations to leverage EDI 278 for streamlined prior authorization. Seamlessly integrating EDI 278 transactions, Astera EDIConnect delivers cost savings, faster response times, and reduced administrative burden.
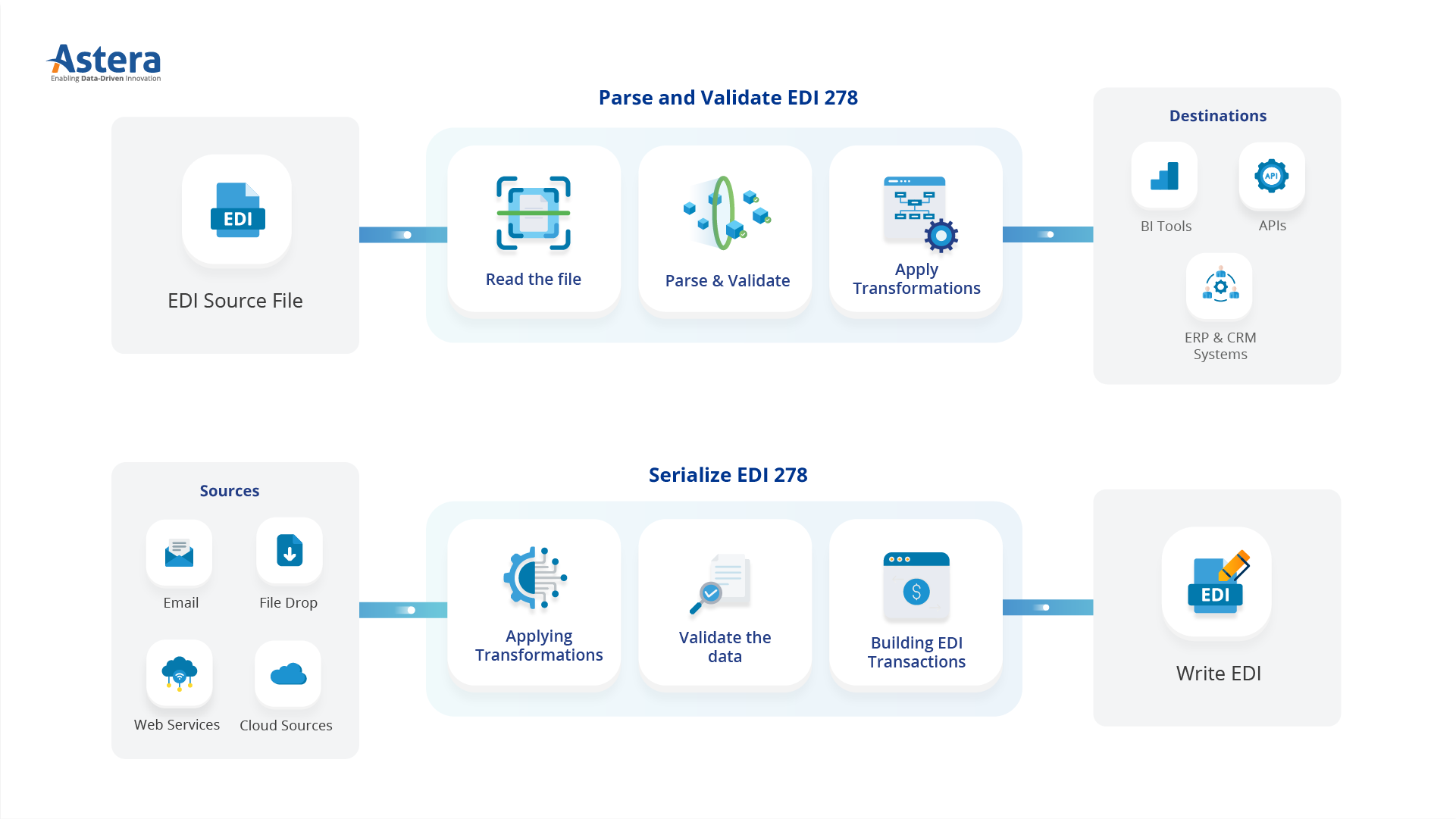
How Astera simplifies EDI 278 workflows to streamline prior authorization
Astera EDIConnect offers:
- Data Translation and Mapping: Simplify data exchange by automating translation and mapping between different EDI formats, ensuring accurate communication with trading partners and reducing errors.
- Validation and Compliance: Ensure data accuracy and compliance by performing real-time validation checks against industry standards and trading partner specifications, minimizing errors, improving data integrity, and meeting regulatory requirements.
- Secure Communication: Safeguard sensitive patient information through secure communication protocols and ensuring compliance with data security regulations.
- Seamless Integration with Provider Systems: Seamlessly integrate with existing provider systems, such as EHR and prior authorization software, eliminating manual data entry, reducing administrative burdens, and enhancing operational efficiency.
- Real-time Updates and Communication: Enable real-time updates, prompt decision-making, and efficient coordination between providers and payers. Receive timely authorization responses, track authorization status, engage in real-time communication, and receive alerts and notifications for any changes in the authorization process.
Streamline your prior authorization process with EDI 278 and Astera EDIConnect. Join our demo session and see how you can benefit from faster, accurate, and secure data exchange between providers and payers. Improve patient care and financial outcomes with lower costs, quicker responses, and fewer denials.
 Astera AI Agent Builder - First Look Coming Soon!
Astera AI Agent Builder - First Look Coming Soon!