Efficient medical claims processing is crucial for timely patient care and financial stability in healthcare. Processing claims swiftly and accurately ensures that healthcare providers receive prompt reimbursements, enabling them to maintain services, invest in staff training, and acquire advanced medical technologies.
Astera is an advanced data extraction solution that is specifically designed to handle complex data extraction tasks, such as medical claims processing. It’s engineered to convert unstructured data, often found in medical claim forms, into structured, actionable information.
Furthermore, Astera has an intuitive and user-friendly interface that allows users to ingest data from various sources, define extraction rules, and specify output formats without writing code.
This makes it an ideal tool for healthcare providers and insurance companies who need to extract data from medical claims for analysis but do not have a technical background. Therefore, our solution expedites the claim settlement cycle, enhances operational efficiency, and benefits patients by facilitating quicker access to necessary healthcare services.
Example Use Case: Medical Claims Processing
An insurance organization processes hundreds of medical claims daily. Various healthcare providers submit these claims, each presenting crucial data such as patient details, diagnosis codes, and treatment procedures in unique formats. Traditionally, the administrative staff manually extracts this data, a process that is time-consuming and susceptible to human errors.
Astera offers an automated and efficient solution to these challenges.
With its rich set of features tailored for handling the complexities of medical claims data, it simplifies and automates the data extraction process. The solution enables the configuration of specific extraction parameters, allowing the system to intelligently identify and pull relevant information from various document types, including:
- PDFs.
- Excel sheets.
- Or even scanned documents.
By choosing Astera, insurance organizations can significantly reduce the risk of errors and improve the claims processing time, thereby improving its overall efficiency and service quality.
A Step-By-Step Guide to Streamlining Claims Processing
As a large-scale insurer processing a substantial volume of medical claims daily, you encounter challenges with claims submitted by different healthcare providers containing critical data in diverse formats. You’re looking for a solution to efficiently extract, process, and analyze this data to expedite claims processing.
Here’s how you can use Astera’s data stack to streamline your medical claims processing:
1. Receiving Claims
The process starts when you receive healthcare claims on a regular basis from various healthcare providers. Each claim is a unique document, rich with vital information that needs to be accurately processed. These claims are promptly stored in a dedicated folder upon receipt.
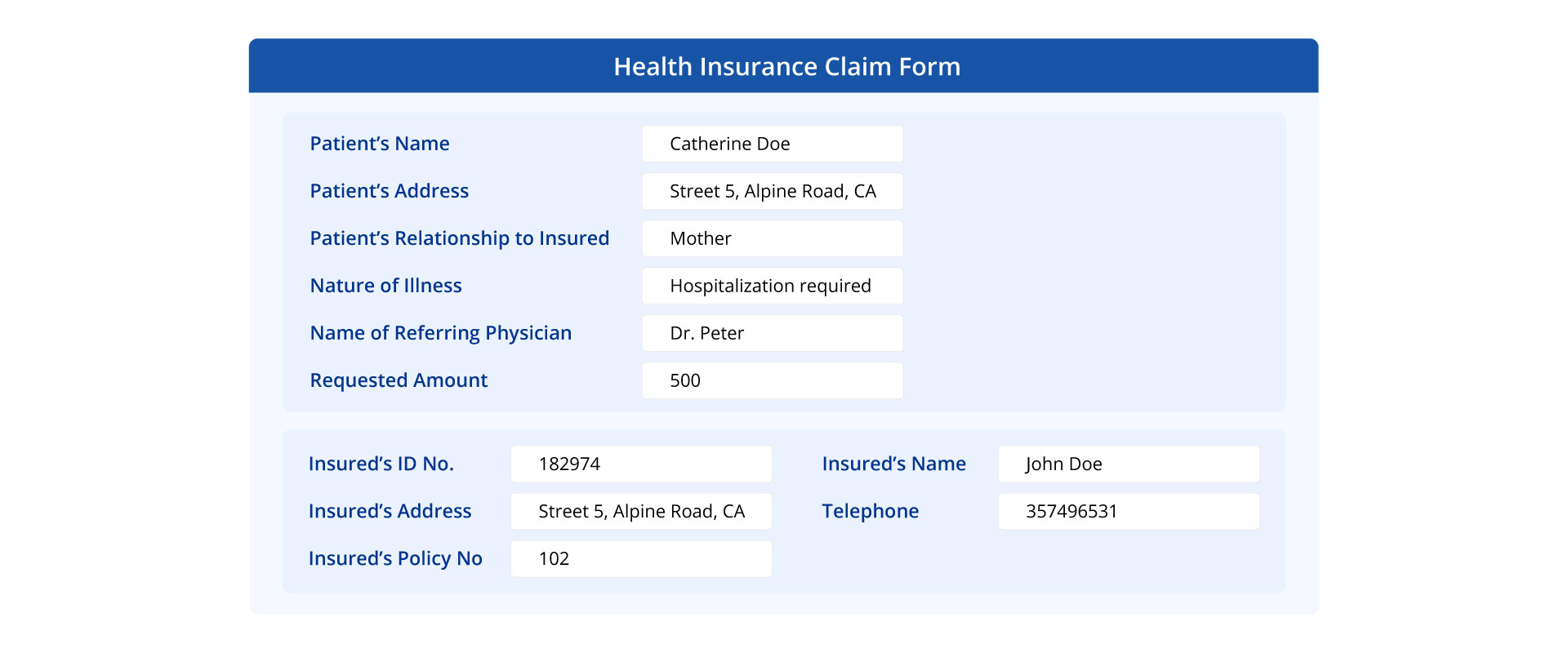
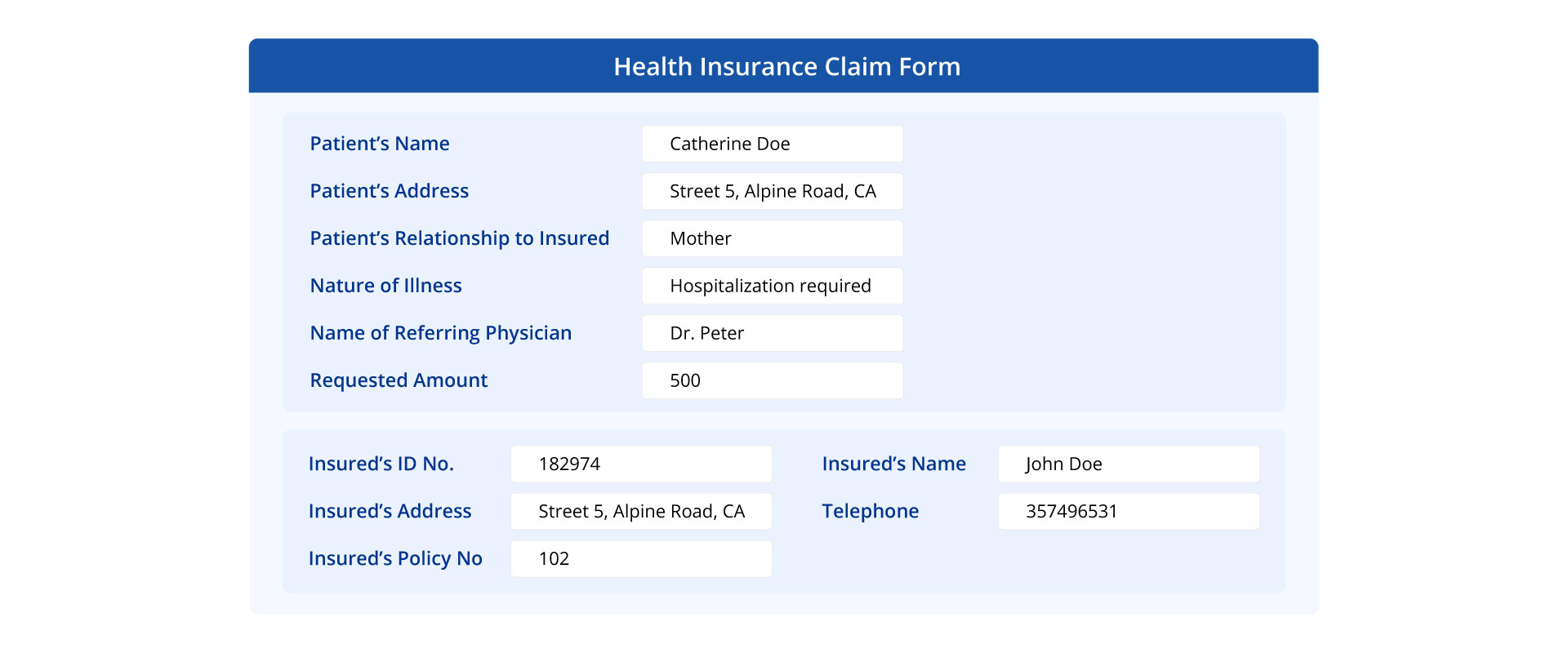
Healthcare Insurance Claim Form in PDF Format
2. Data Extraction
Next, you can use Astera to automate the extraction of relevant data from these claims. Astera’s AI recommended layout feature allows you to automatically generate models for multiple source files at once. This can be achieved by specifying the data layout that needs to be extracted from the document, which can be done manually, through an existing Astera artifact, or in JSON format. This feature, coupled with its ability to handle different formats and complex hierarchical data structures, ensures accurate and efficient data extraction.
Automating data extraction using Astera
3. Data Verification and Validation
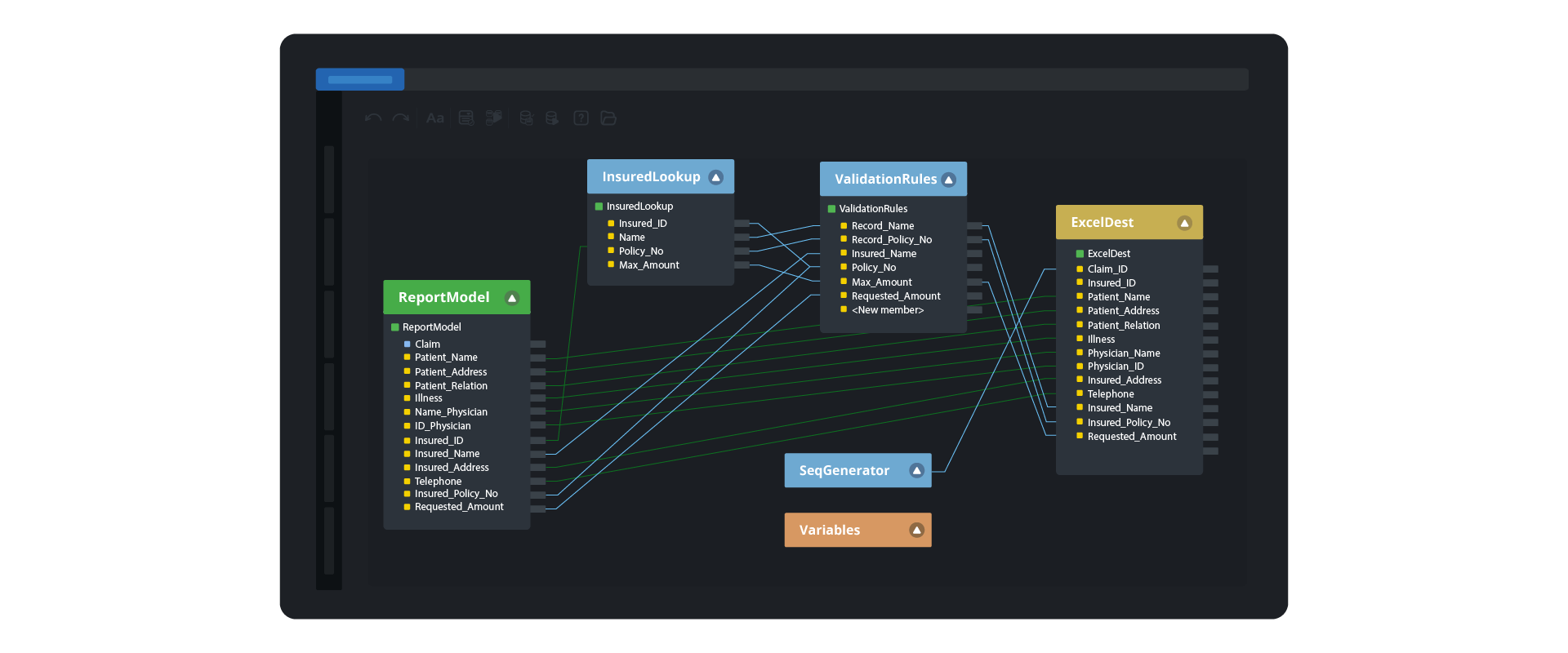
After the data is extracted, it is ready for validation. By employing the report model as a source within dataflows, you can effortlessly utilize Astera to ensure the accuracy, consistency, and integrity of the data through rigorous validation and verification processes tailored to meet its specific requirements.
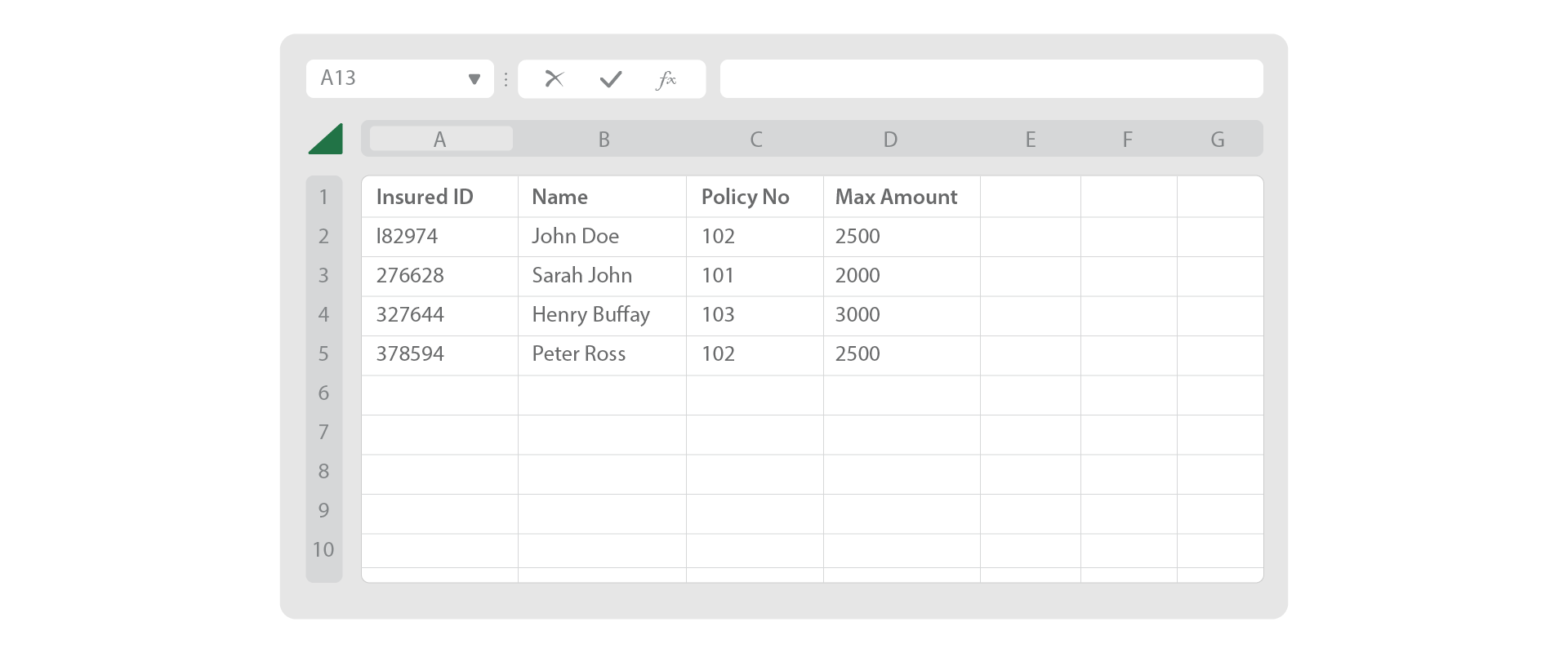
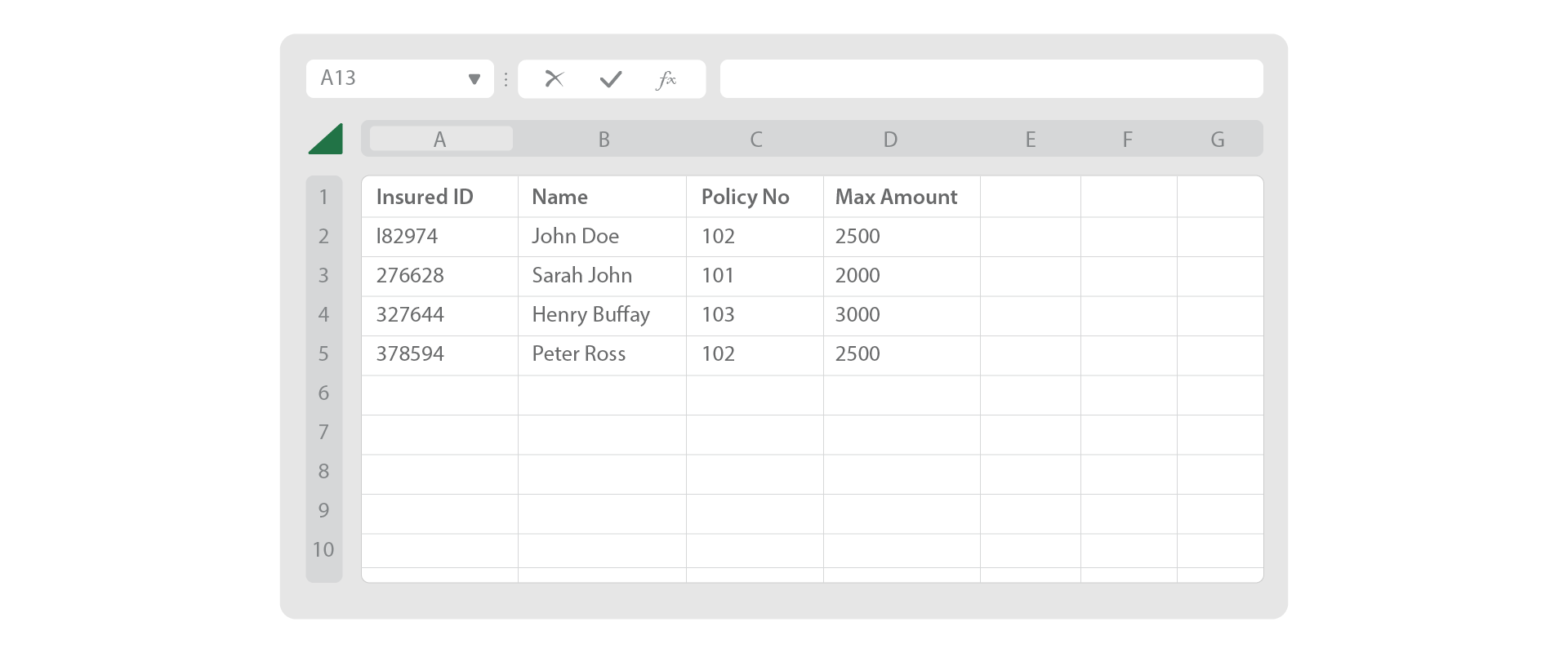
Verifying details from the insurer’s database
Key steps in this phase include cross-verifying insurer details in the claim form with the company’s database, validating the requested claim amount against policy limits, and generating a unique claim ID for each new record.
Data transformations in Astera
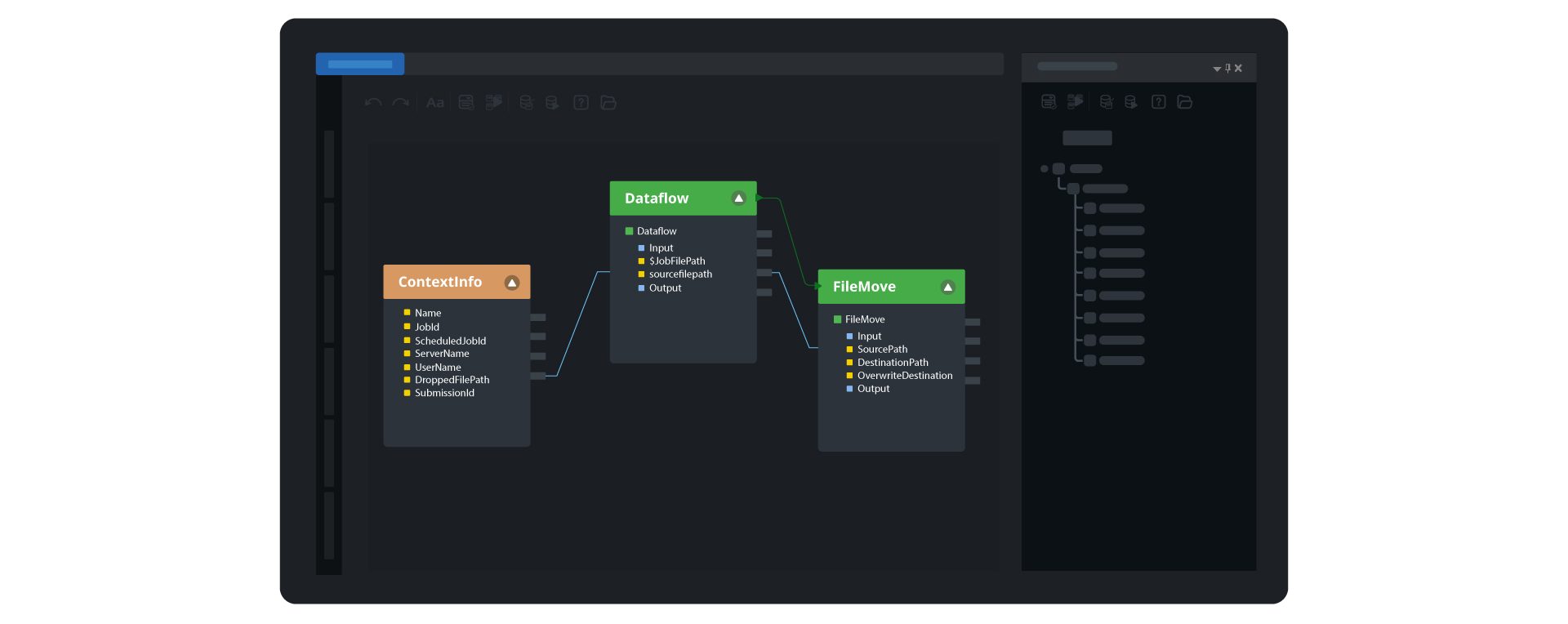
4. Workflow Automation
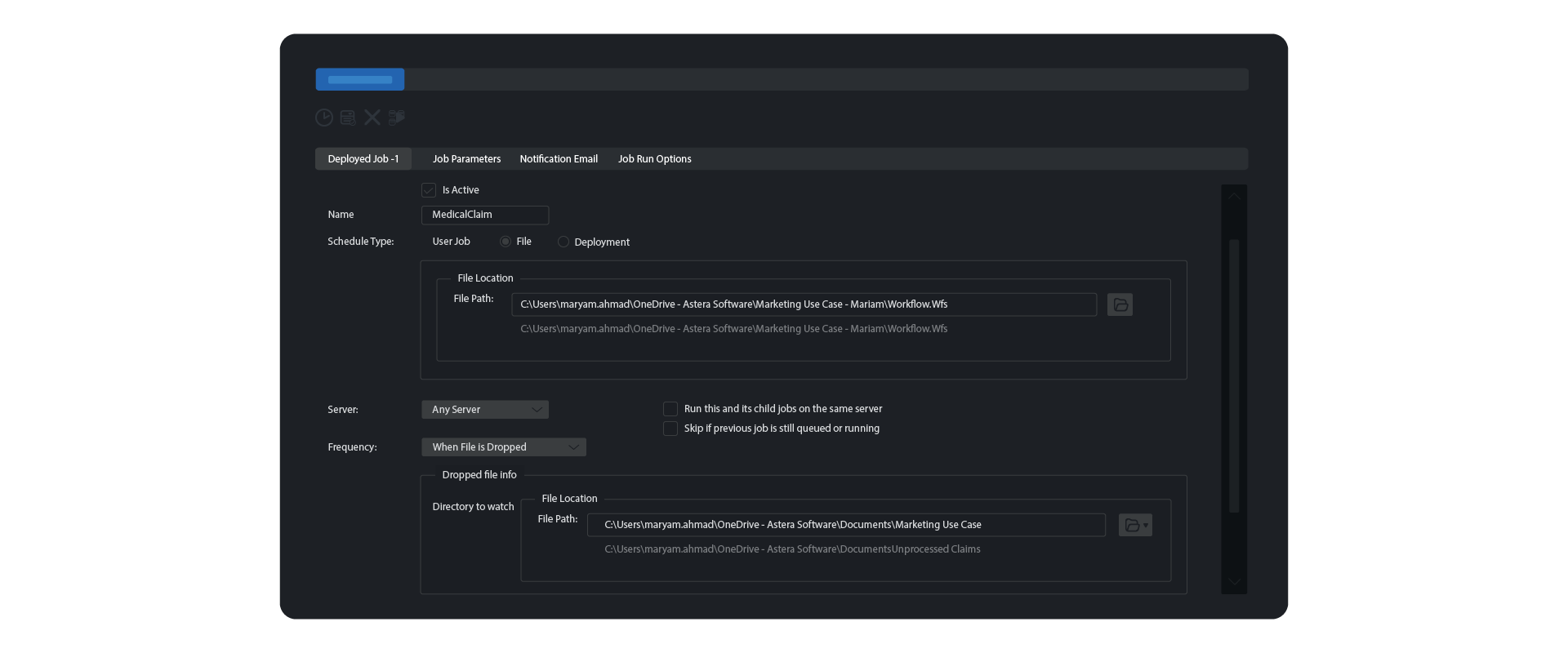
The final step involves automating the entire workflow. Upon detection of a new claims file in the directory where all our unstructured claims appear, the dataflow, configured to use the source file path information, initiates real-time data extraction and transformation. Once processed, the file is moved to a designated folder, ensuring an organized workflow.
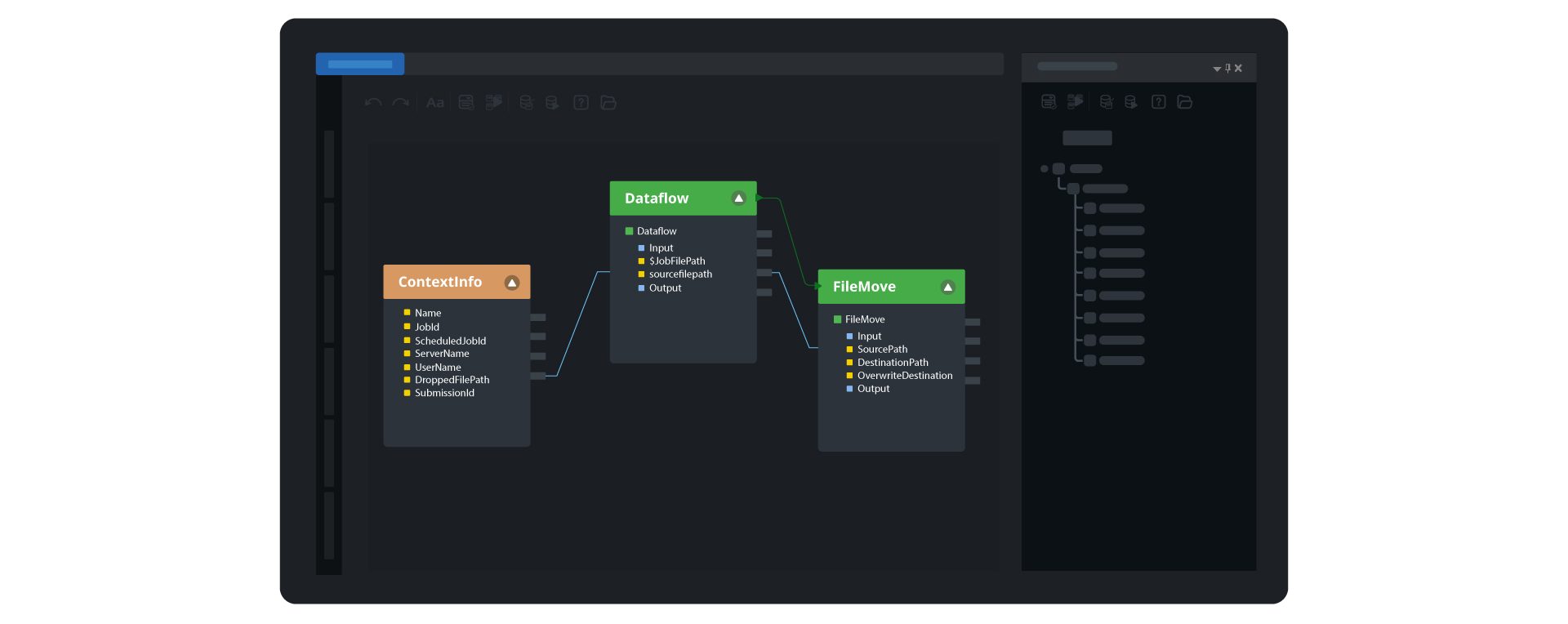
To maintain efficiency, a scheduler is deployed to monitor the directory for unprocessed claims. Astera’s file drop automation feature ensures that the arrival of a new file automatically triggers the workflow, eliminating manual intervention and enhancing the overall efficiency of the claims processing operation.
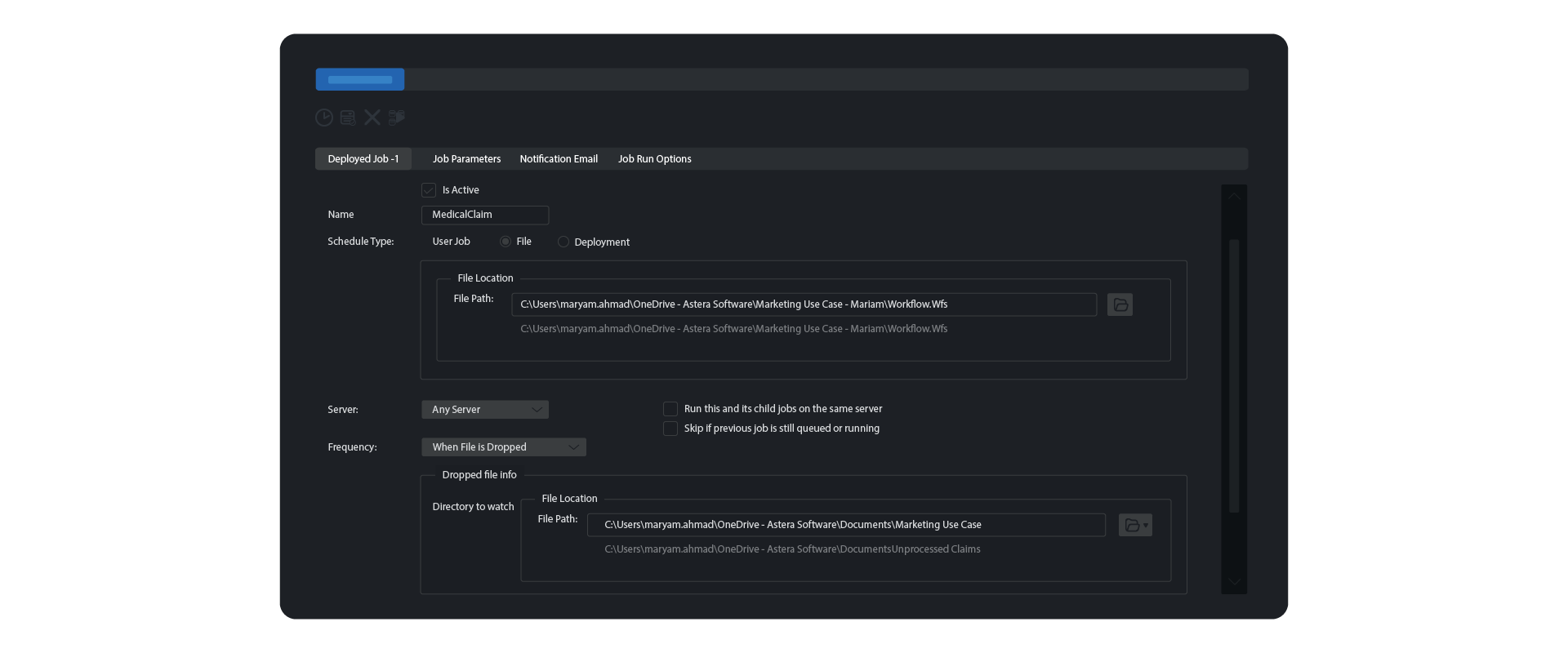
Scheduling claims file drop automation in Astera
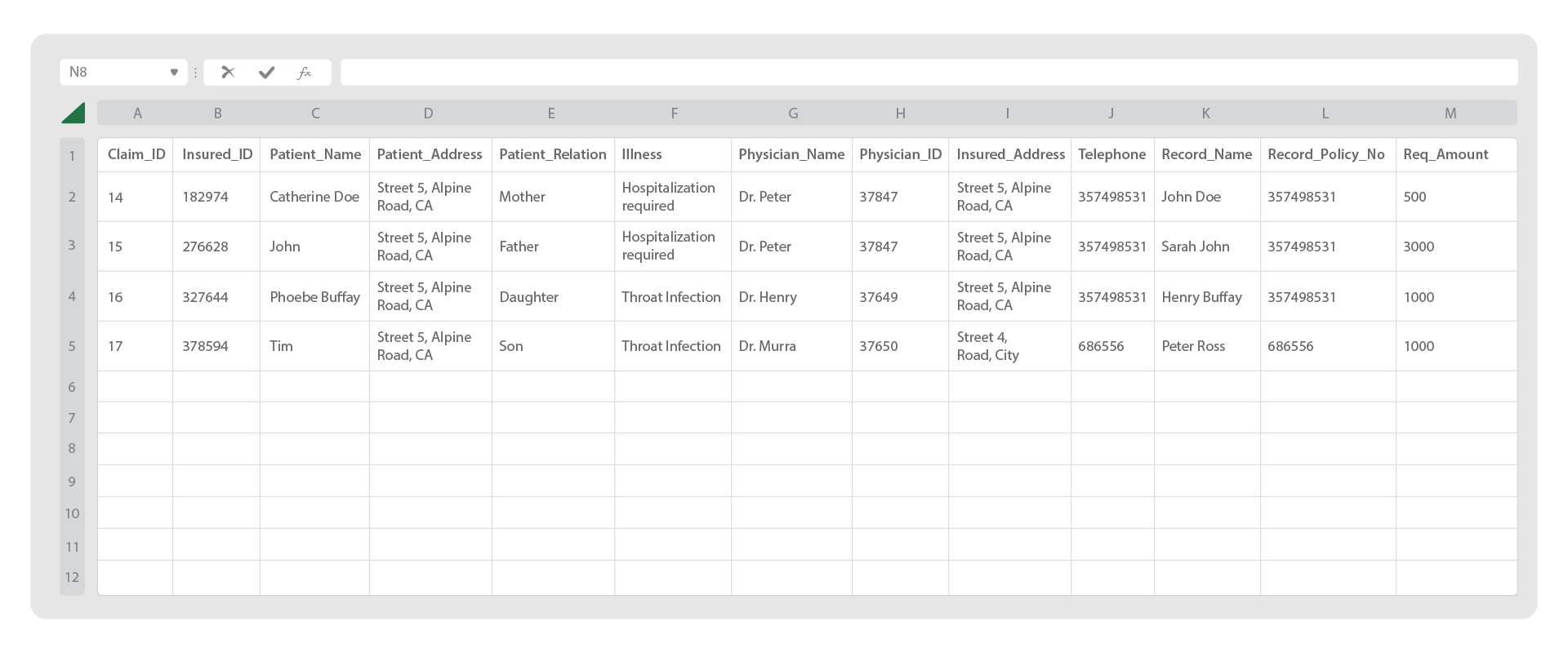
Utilizing Astera’s unstructured data extraction solution, each claim is processed in real time, ensuring all claim records are swiftly and accurately added to the repository.
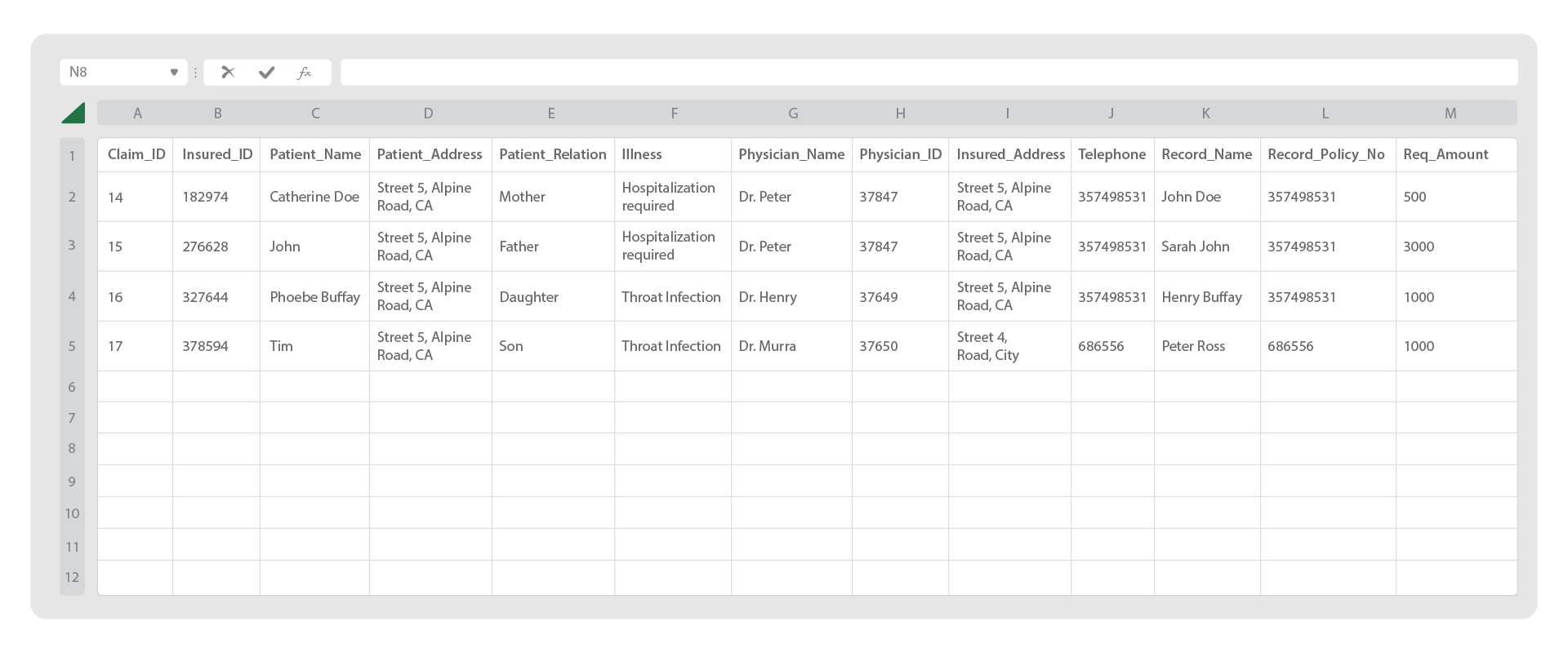
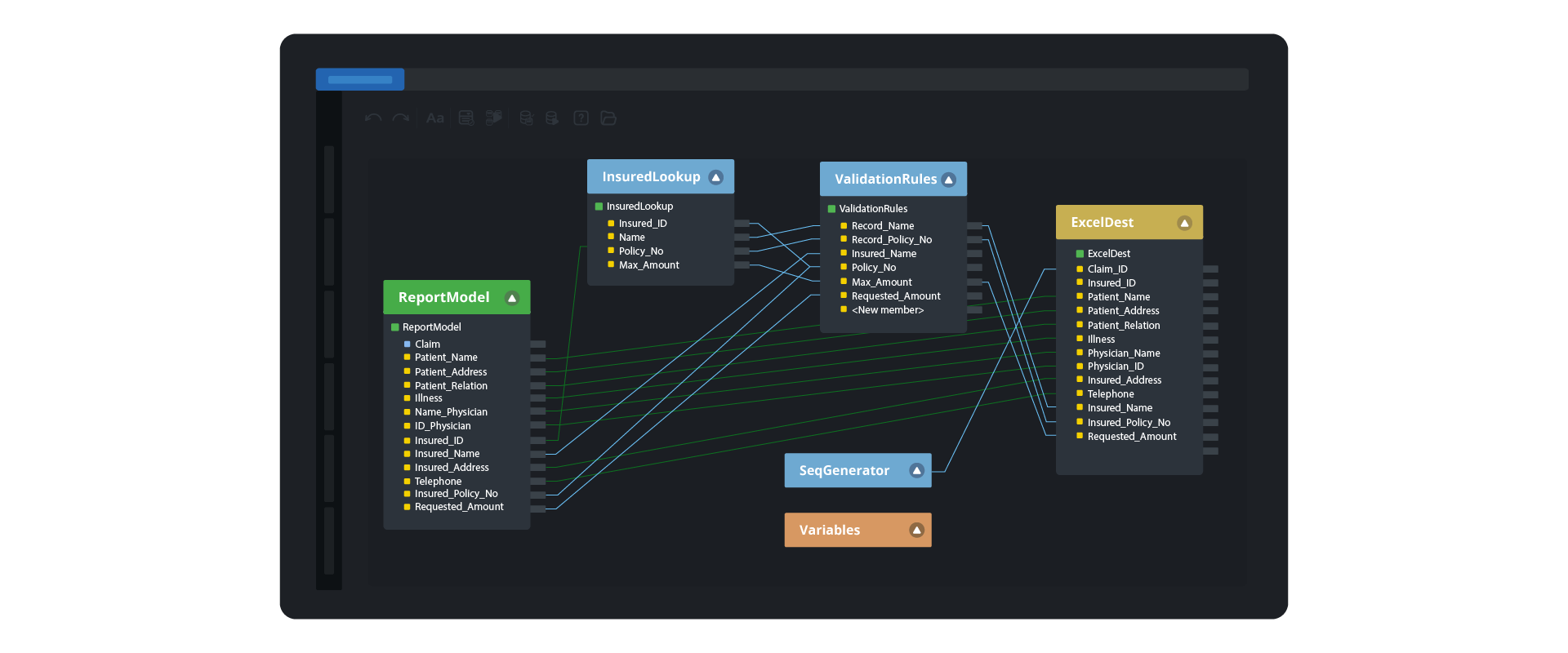
Medical claims data is consolidated in an Excel File
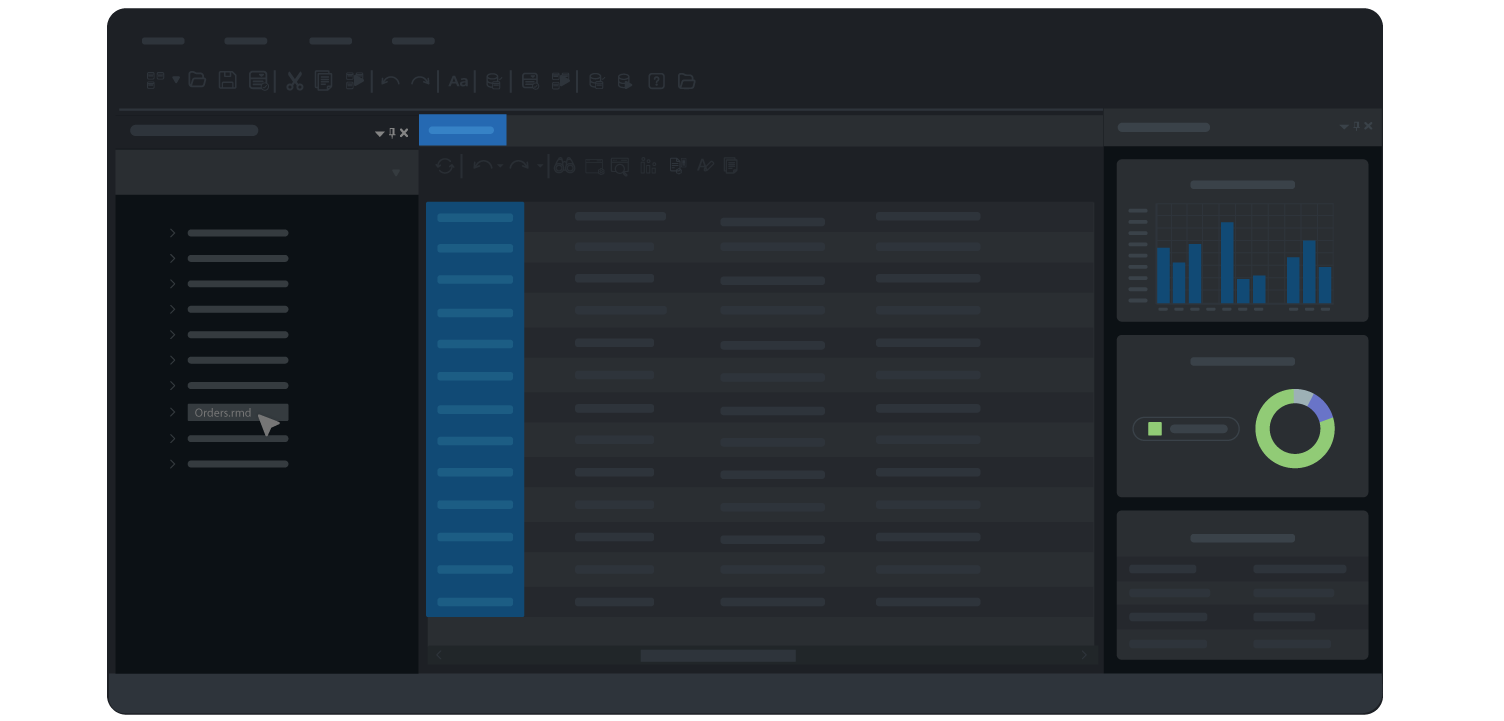
On structured, consolidated claims records, you can leverage Astera’s advanced data preparation capabilities to prepare it for analysis. This involves cleansing the data to remove any inaccuracies, filling in missing values, and eliminating duplicates. Astera provides instant data preview, allowing you to modify and monitor the data in real-time. Moreover, its profile browser, displayed as a side window, allows you to assess the data’s health, ensuring that it is clean, accurate, and ready for analysis.
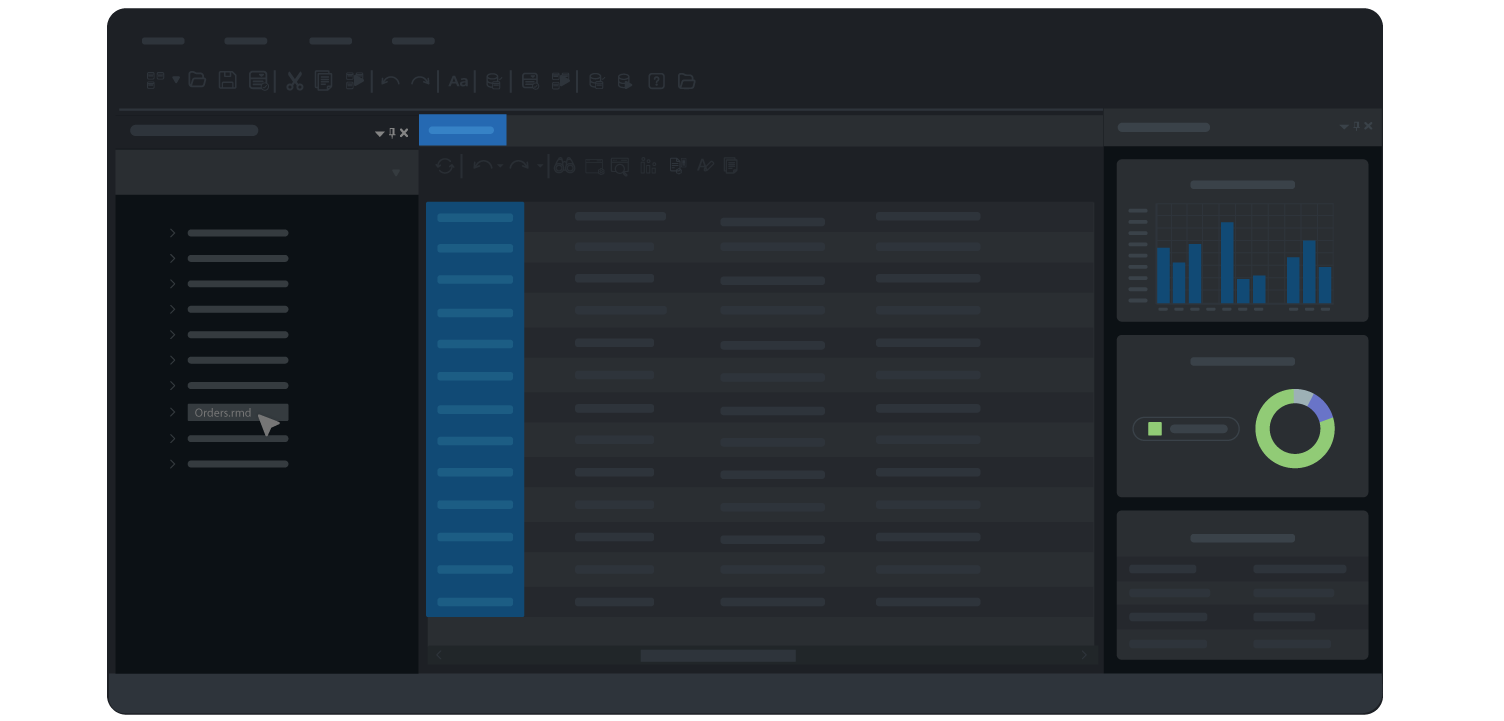
Data profiling and preparation using Astera
Benefits of Astera in Medical Claims Processing
Astera offers many benefits that significantly simplify the process of medical claims processing:
Automation:
Astera plays a pivotal role in automating the data extraction process within medical claims processing, reducing the reliance on manual efforts. By streamlining the handling of diverse medical data formats, the tool introduces efficiency into a traditionally time-consuming task, allowing healthcare organizations to process claims with greater speed and accuracy.
Enhanced Accuracy:
The intelligent extraction capabilities of Astera significantly enhance the accuracy of medical claims processing. The tool is adept at precisely identifying and retrieving relevant information from various document types, minimizing the risk of errors that could impact the integrity of critical data points, including patient details, treatment histories, and billing codes.
Efficiency Gains:
Astera contributes to efficiency gains by accelerating the overall claims processing timeline. This not only expedites the reimbursement cycle but also frees up valuable resources that would otherwise be dedicated to manual data entry. The result is a more streamlined and resource-efficient workflow for healthcare providers.
Time Savings:
The rapid and consistent data extraction facilitated by Astera translates into significant time savings for healthcare organizations. The automation of labor-intensive processes enables staff to allocate their time more strategically, focusing on tasks that require human expertise and contributing to a more effective and agile healthcare environment.
Adaptability:
Astera’s adaptability to diverse data formats commonly encountered in the healthcare sector, including PDFs, Excel sheets, and scanned documents, underscores its versatility. By ensuring seamless integration with existing systems, Astera proves to be a robust solution that aligns with the dynamic nature of medical claims data and supports the interoperability of various data sources.
Final Word
Astera is a powerful tool that empowers healthcare providers to streamline their medical claims processing. Its suite of features, including automated data extraction, advanced pattern recognition, and AI-recommended layouts, are designed to enhance productivity, ensure accuracy, and simplify workflows.
By reducing manual effort, minimizing errors, and accelerating claims processing times, Astera allows healthcare providers to focus on what truly matters — delivering quality patient care. Take the first step towards a more efficient and effective medical claims processing system with Astera by downloading its free 14-day trial today.
Experience Hassle-Free Medical Claims Processing with Astera ReportMiner
Unlock the power of automated data extraction with Astera ReportMiner. Simplify your medical claims processing, reduce errors, and save valuable time. Try Astera ReportMiner free for 14 days and see the difference it can make.
Start Your Free 14-Day Trial Authors:
 Mariam Anwar
Mariam Anwar



 March 27th, 2025
March 27th, 2025