
EDI 270 Eligibility, Coverage or Benefit Inquiry Transaction Set
The Health Insurance Portability and Accountability Act (HIPAA) requires health insurers to follow Electronic Data Interchange (EDI) standards for healthcare. The EDI 270 transaction set, or the ANSI X12 270, verifies a patient’s insurance eligibility, coverage, and benefits. It can also check whether an individual is eligible for a specific government healthcare program like Medicare.
What is the EDI 270 Eligibility, Coverage, or Benefit Inquiry Transaction Set?
The EDI transaction enables healthcare providers, such as hospitals, clinics, or physicians’ offices, to electronically request and receive detailed Information about a patient’s insurance coverage from the patient’s insurance payer.
Key Data Elements in EDI 270 Transaction Set
The EDI 270 transaction set contains five key data elements, each serving a specific purpose in the inquiry process:
- Patient Identification includes the patient’s name, date of birth, and other identifiers such as patient ID or social security number (SSN). These details help with accurate patient identification within the insurance payer’s system.
- Provider Information identifies the healthcare provider inquiring, including name, address, and provider ID. It helps the insurance payer direct the response to the correct provider.
- Payer Information specifies which insurance company or payer to request coverage and benefit information from. It includes the payer’s name, ID, and other necessary identifiers.
- Service Date indicates the date for which eligibility and benefit information is needed. This is the date of service or the anticipated date of service.
- Additional Information may include specific questions about eligibility status, coverage details (such as co-pays and deductibles), and any other pertinent benefit information the provider requires.
Process of an EDI 270 Transaction
When a healthcare provider initiates an EDI 270 transaction, it goes through the following steps:

-
Preparation
The provider prepares and sends an EDI 270 transaction using their healthcare information system (HIS) or practice management system (PMS). The transaction is formatted according to the ANSI X12 standard, ensuring compatibility with the payer’s systems.
-
Transmission
The EDI 270 transaction is transmitted securely to the designated insurance payer through a secure network, such as a clearinghouse, or directly to the payer’s EDI gateway.
-
Processing
Upon receipt of the EDI 270 transaction, the insurance payer’s system processes the inquiry. It validates the request against its database to verify patient eligibility and retrieves detailed benefit information associated with the patient’s coverage plan.
-
Response
The insurance payer generates an EDI 271 transaction in response to the provider’s inquiry. The EDI 271 transaction confirms the patient’s eligibility status and outlines coverage details.
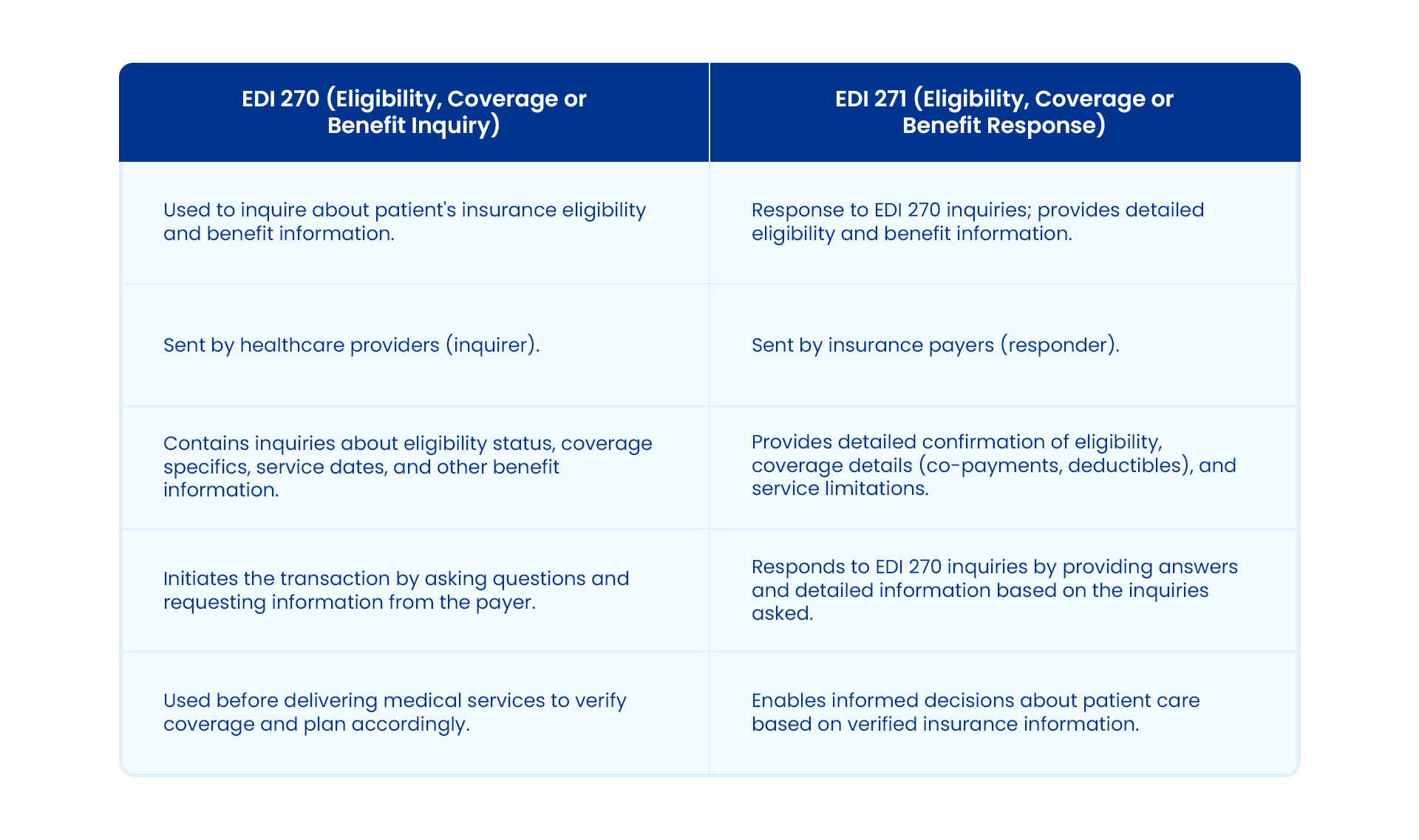
EDI 270 vs. EDI 271
The EDI 270/271 transaction works as a pair and functions as a question-and-answer mechanism. However, a few differences differentiate EDI 270 from EDI 271.
EDI X12 270 File Format Sample
This document is divided into functional groups that explain the contents of the transaction. A typical EDI 270 document looks like this:
ST*270*1234*005010×279~
BHT*0022*13*10001234*20101115*1319~
HL*1**20*1~
NM1*PR*2*BMCHP*****46*04337331~
HL*2*1*21*1~
NM1*1P*1*ITIS*ARTHUR*MD***XX*1234567890~
REF*N7*234899~
N3*39 DALTON STREET~
N4*BOSTON*MA*02199~
PER*IC*CHARLEY HORSE*TE*6175551212*EX*2805*FX*6175551213~
HL*3*2*22*1~
NM1*IL*1*TRIPPER*JACK*T***MI*111223303~
REF*1L*599119~
N3*29 JETPORT ROAD~
N4*CAMBRIDGE*MA*02138~
DMG*D8*19510519*M~
DTP*291*D8*20160630~
HL*4*3*23*0~
TRN*1*93175-012547*9877281234*RADIOLOGY~
NM1*03*1*TRIPPER*JACQUES~
REF*SY*003221234~
DMG*D8*20061014*F~
DTP*291*D8*20160630~
EQ*30**FAM~
SE*25*1234~
EDI 270 Specification and File Components
The EDI 270 specification outlines the necessary components for constructing a valid eligibility inquiry transaction. This transaction set utilizes these key components to facilitate seamless data exchange:
- The ISA and GS segments for sender and receiver identification.
- ST and BHT segments that initiate and define the transaction type and hierarchy.
- The HL segment establishes hierarchical relationships (e.g., patient, provider).
- NM1 segments identify entities involved, and TRN segments provide tracking Information.
- DMG segments capture detailed demographic data, and DTP segments manage date/time specifics.
- EQ segments describe equipment characteristics related to the inquiry, ensuring complete information exchange for patient care planning.
This structured approach streamlines administrative processes and enhances accuracy in determining patient coverage and benefits before service delivery.
Use Case: The Exchange of EDI 270/271 Transactions
Let’s consider an example use case. A patient schedules a routine checkup appointment with a healthcare provider. Before providing services, the provider initiates an EDI 270 transaction to verify the patient’s insurance coverage with Alpha Insurance Company, a fictional insurance firm. This transaction includes details about the patient, the healthcare provider, and the requested services.
Upon receiving the EDI 270 inquiry, Alpha Insurance Company processes the request and sends an EDI 271 response. The EDI 271 transaction confirms or denies the patient’s coverage, outlines the specific benefits, including any co-pays or deductibles, and provides other relevant policy information. This electronic exchange eliminates the need for manual verification, reduces administrative burdens for the provider and the payer, and ensures timely patient care.
Simplify Business Transactions with Astera EDIConnect
The EDI 270 transaction set helps healthcare providers streamline verifying patient insurance coverage and benefits. By electronically exchanging EDI 270/271 transactions, healthcare providers and payers can ensure accurate and timely Information.
Astera EDI Connect offers a solution for seamless automation of EDI messages, including ANSI X12 standards. By leveraging Astera, users can automate the creation and transmission of EDI 270 inquiries to health insurance payers, eliminating the need for manual coding.
The user-friendly solution ensures seamless payment communication using secure protocols like AS2 and SFTP. Astera EDI Connect automates the processing of EDI 271 response messages and workflows, reducing the risk of errors and delays.
With real-time transaction monitoring capabilities, Astera empowers its users to promptly identify and address any EDI-related issues, ensuring a smooth verification process.
Want to simplify and automate the EDI 270/271 transactions? Schedule a personalized demo now to improve EDI transaction efficiency and deliver quality care to patients.
 Astera AI Agent Builder - First Look Coming Soon!
Astera AI Agent Builder - First Look Coming Soon!

