
EDI 835 Health Care Claim Payment/Advice
What is an EDI 835?
Organizations use Electronic Data Interchange (EDI) to communicate electronically with their partner organizations. EDI 835, also known as Health Care Claim Payment/Advice, is an electronic file format used to transmit healthcare claim payment information. This transaction set is used to make payments to healthcare providers and provide Explanations of Benefits (EOB). An EDI 835 document is organized into data elements and segments which include information, such as what charges were paid, mode of payment, and deductible amount.
This electronic data exchange occurs between healthcare organizations, insurance companies, and clearinghouses. The fact that it standardizes the exchange of payment details ensures seamless communication and a significantly reduced need for manual processing.
What components does an EDI 835 file have?
An EDI 835 file consists of several segments, each serving a specific purpose. Here are the key components you’ll find in an X12 EDI 835 file:
- Header Segment: Contains general information about the file, such as sender and receiver identifiers, transaction type, and creation date.
- Provider Level Adjustment: Provides details about any adjustments made at the provider level, such as contractually obligated discounts or refunds.
- Patient Level Adjustment: Specifies adjustments made at the patient level, such as co-pays or deductibles.
- Service Line Information: Contains detailed information about each service rendered, including dates, charges, and payment amounts.
- Claim Level Adjustments: Describes any adjustments made at the claim level, such as penalties or rejections.
- Summary Segment: Summarizes the financial details of the entire payment advice, including total payment amounts and check numbers.
- Footer Segment: Concludes the EDI 835 file, often with control totals and additional administrative information.
EDI 835 example
To better understand EDI 835, let’s consider an example. Suppose a healthcare provider submits a claim for payment to an insurance company. The insurance company processes the claim and generates an EDI 835 file to communicate the payment details to the healthcare provider. This EDI file would contain information such as the patient’s name, service dates, charges billed, and allowed amounts.
Upon receiving the EDI 835 file, the healthcare provider’s system processes the file, extracting and interpreting the relevant information. This is what an EDI 835 file looks like:
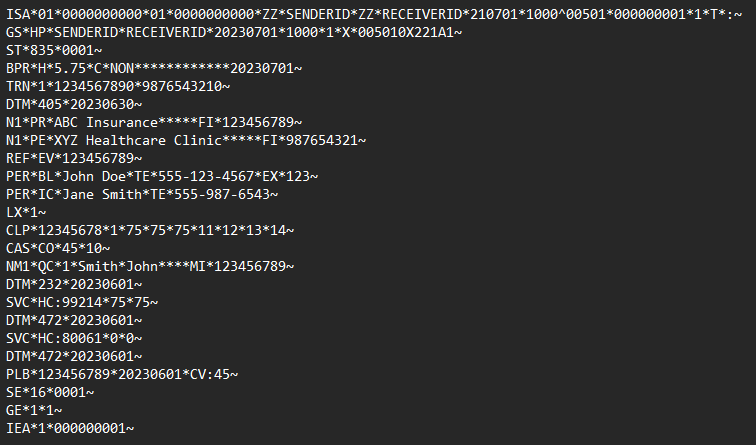
Note: This is only an example EDI 835 file. It does not reflect the exact content or structure of real-world EDI 835 messages.
To acknowledge the receipt of the EDI 835 file, the healthcare provider may send an EDI 997 (Functional Acknowledgment). EDI 997 is a standard acknowledgment EDI that confirms the receipt of the EDI file. However, it does not mean that the trading partner agrees with the contents of the EDI file. So, in this case, it only informs the insurance company that the healthcare provider’s system successfully received the file without any transmission errors.
What are the benefits of EDI 835?
Implementing EDI 835 offers numerous advantages for all parties involved in healthcare claim processing:
- Automation and Efficiency: EDI 835 eliminates manual data entry and reduces paper-based processes, leading to faster and more accurate payment reconciliation.
- Cost Savings: By minimizing paperwork, EDI 835 significantly reduces administrative costs associated with claim processing, postage, and storage.
- Enhanced Accuracy: The standardized format of EDI 835 reduces the risk of errors and discrepancies in payment information, ensuring greater accuracy and reducing payment delays.
- Faster Reimbursement: EDI 835 expedites the payment cycle, allowing healthcare providers to receive payments more quickly and efficiently.
- Improved Visibility: With detailed payment information available in a structured format, providers can easily track and reconcile payments, improving financial visibility and decision-making.
How can I use EDI 835?
The EDI 835 transaction set is one of the most commonly used transaction sets in the healthcare industry. Information requested in an EDI 837 (Health Care Claim: Professional) transaction is transmitted using the EDI 835. To leverage the benefits of EDI 835, you need an EDI solution that supports the required format. This generally entails adopting an EDI solution or collaborating with a reliable EDI service provider. Here’s a general overview of the steps involved:
- Set up an EDI system: Choose an EDI software and partner that offers EDI capabilities, specifically for handling EDI 835 files.
- Integration: Integrate the EDI system with your existing healthcare information systems, such as billing or practice management software.
- Mapping and Translation: Ensure that your EDI system can accurately map and translate the EDI 835 files into a format compatible with your internal systems.
- Validation and Processing: Validate incoming EDI 835 files for errors, process the data, and apply it to your payment reconciliation workflows.
- Reporting and Analytics: Leverage the data from EDI 835 files to generate comprehensive reports, gain insights, and make informed business decisions.
How Astera EDIConnect helps
EDI has revolutionized the way healthcare claim payments are handled, bringing efficiency, accuracy, and cost savings to the industry. Healthcare providers can streamline payment processing and improve financial visibility by leveraging a powerful EDI solution.
Astera EDIConnect is a robust and flexible EDI solution that simplifies your EDI 835 processing. It offers:
- Built-in EDI parser, validator, and transaction builder
- Seamless integration with your existing systems.
- Automated mapping and translation of EDI 835 files.
- Robust validation and error handling capabilities.
- Industry-standard compliance.
It also supports X12 and EDIFACT standards, enabling you to exchange various transaction sets, including EDI 835, with your trading partners seamlessly.
 Astera AI Agent Builder - First Look Coming Soon!
Astera AI Agent Builder - First Look Coming Soon!


